For patients attending the eye clinic or local optician, the eye assessment often includes the dreaded eye pressure check. This can often include the air puff tonometer, a device that applies a small jet of air towards the eye. In my experience, patients often find this very uncomfortable. In an eye clinic setting, Ophthalmologists often use an ‘applanation tonometer’. This technique involves the use of local anaesthetic in the eye, and the manual checking of the eye pressure. Whilst it is more accurate, readings are limited to the time of day, actual device and clinician performing the measurement (so called inter-observer variability).
The problem we have as Glaucoma specialists is that pressure readings are vital to know whether the condition is being managed satisfactorily. In this context, we only obtain a pressure reading when the patient attends the clinic, and so we have no knowledge of what the eye pressure is doing in between appointments, at other points of the day and at night.
Future methods for checking the eye pressure:
Contact lens
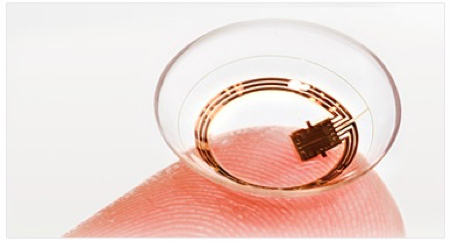
New contact lens sensors are now becoming available for patients. These measure very small changes in pressure by assessing minimal alterations in the curvature of the cornea. measure small changes in the curvature of the cornea (the clear window of the eye). Some of these lenses can measure for 30 seconds every 5 minutes, producing 86,400 readings over a 24-hour period. The best readings are filtered and the lens produces 300 or so readings per day. This can prove vital for specialists looking to closely monitor a patients’ condition, and represents an improvement on the usual 1 reading every 3 or 4 months that is taken with conventional care. By looking at trends, the specialist can then identify an optimal time for the patient to take their glaucoma medications.
The Triggerfish Contact Lens (courtesy of Sensimed Technologies)
Who would be suitable for a contact lens pressure sensor?
- Potentially all patients who have been diagnosed with with glaucoma and is on treatment require monitoring.
- Patients with a family history of glaucoma, even if your pressures are normal.
- Patients being monitored as glaucoma suspects
- Patients diagnosed with ‘Narrow anterior chambers’ (a condition which can lead to sudden spikes in IOP especially overnight)
Summary of the potential benefits of contact lenses:
- ‘Non-invasive’ and convenient, with no puffs of air or discomfort
- Monitoring IOP continuously up to 24 hours
- Eye pressure is checking all of the time (including at night)
- Enables early diagnosis and personalized treatment
- Prevents future glaucoma damage
Summary of the potential benefits of contact lenses:
- ‘Non-invasive’ and convenient, with no puffs of air or discomfort
- Monitoring IOP continuously up to 24 hours
- Eye pressure is checking all of the time (including at night)
- Enables early diagnosis and personalized treatment
- Prevents future glaucoma damage
Pressure sensing devices within the eye

Developed by Launchpoint, novel pressure sensors are being developed that are incorporate within the intraocular lens that is implanted during cataract surgery. There are some clear advantages of this approach include a lack of influence of external factors normally affecting IOP measurement. The device transmits data wirelessly to a mobile phone for download, and potential sharing with the glaucoma specialist.
The current pace of technological advancement in this area is staggering, and these products are likely to be commonplace in the not-too-distant future. I have no doubt that these devices will dramatically improve the quality of care for glaucoma patients worldwide, and hope to be offering at least one of these to select patients very soon. Watch this space!











